Photo by jesse orrico on Unsplash
Covid-19 is also doing long-term damage to efforts to find a cure for dementia.
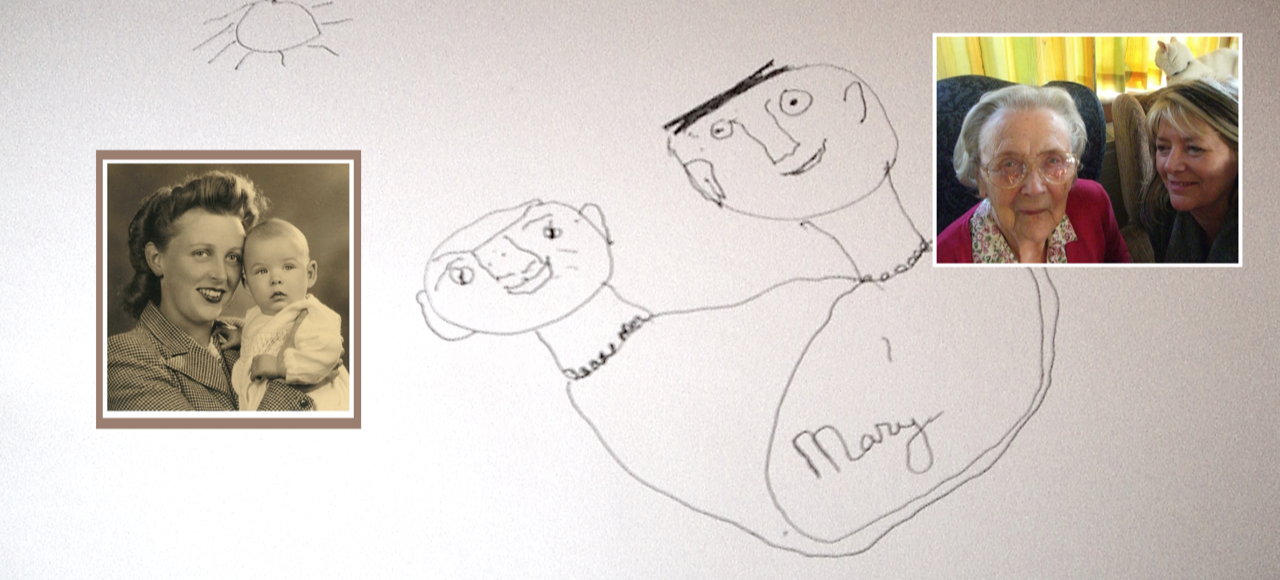
Every day, Diane Evans (not her real name), calls her 85-year-old mother, who lives on her own in Wales from her home in London. Every day she asks her mother if she is remembering to wash her hands regularly and to keep a social distance from other people. Every day, her mother is perplexed by the question.
Every day the facts of life during the coronavirus epidemic are explained to her yet again, with an heroic absence of exasperation.
Every day Ms Evans worries that her mother will put herself at unnecessary risk of contracting the Covid-19 virus.
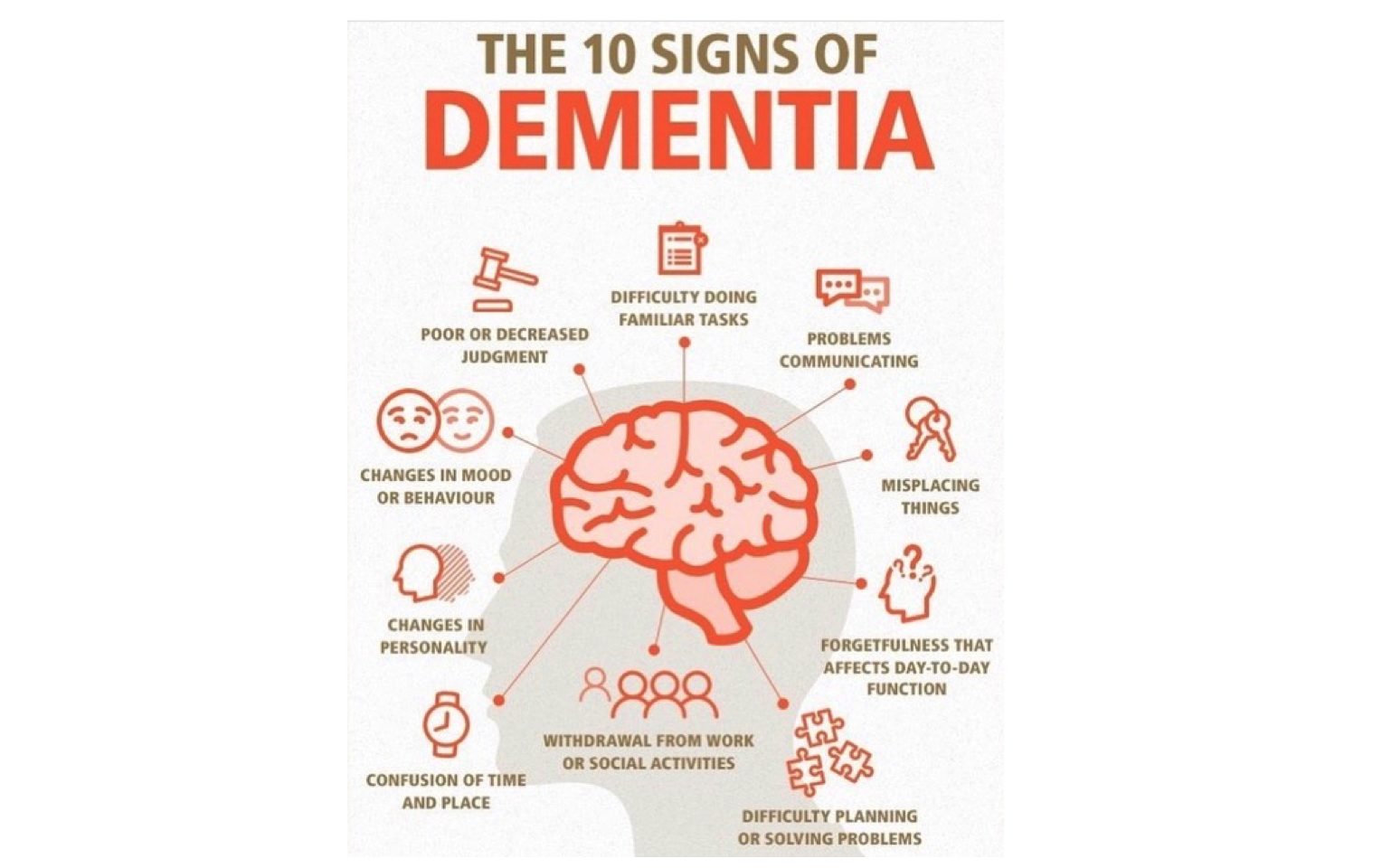
She also worries that the condition her mother already lives with is getting worse, as she loses the social contacts and routine that shaped her life. Her mother has dementia, a degenerative and incurable condition that affects perhaps 850,000 Britons and 50m people worldwide. It has various causes and a wide range of severity. It may start as a “mild cognitive impairment” forgetfulness; the occasional “senior moment”. But as it progresses, it attacks mental agility and gnaws away at memory. Eventually, it renders people incapable of looking after themselves, even if physically they are up to it. They will lose the ability to read, to cook and to shop. They may forget to drink and become dehydrated, or become incontinent. At times they may suffer delusions, or become frightened or angry; at others simply subside into an apathetic slump. They will require care for most of their waking hours, and often supervision when they sleep.
People with every stage of dementia are at particular danger from the virus not just because of the difficulty they may have in understanding the threat or in remembering safety precautions. They are also likely to be subject to other risk factors. The most obvious is that dementia is predominantly a syndrome of the elderly, the group for whom covid-19 is most likely to be fatal. A small minority of people with early-onset dementia develop symptoms in their younger years. But no one doubts that it becomes more common with age. By some estimates, 2% of 65- to 69-year-olds have dementia, and its prevalence doubles every five years to the age of 90. In another widely quoted estimate, between a third and a half of 85-year-olds have dementia.
The condition has a variety of causes. The most common is Alzheimer’s disease, accounting for between 60% and 80% of cases, but there are dozens of other types. And, though all kinds of people in all states of health can develop dementia, it does appear to be correlated with other conditions that make people vulnerable to infection. Those who are overweight, depressed, smoke, have high blood pressure or diabetes and do not exercise have a higher risk of dementia, as well as of physical ailments.
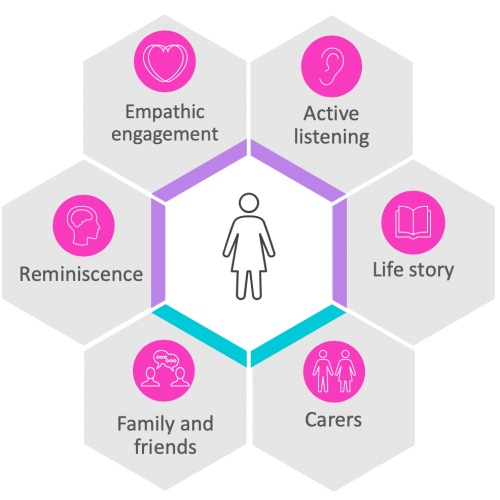
Looking after people with dementia is a hands-on, labour-intensive task. For those at home, that can become almost impossible if social-distancing guidelines are adhered to. And much of the usual support system, regular visitors and day-care centres, for example—will be unavailable.
Technology can help a bit. Singapore, for example, has experimented in some public-housing blocks with a system that sends neighbours or family members of the vulnerable an alert if, say, a tap in a washbasin has not been used for a while. Researchers at the Care Research & Technology Centre at Imperial College in London are working on taking this much further. Infra-red and radar sensors installed in the homes of people with dementia, or devices worn by them as watches or hearing-aid-type brain-scanners can provide data giving early warning signs of trouble.
There are also, of course, apps for dementia. “Refresh Player” and “Refresh Studio”, from a tech firm called How Do I?, offer “personalised memory support”, including videos on how to perform day-to-day tasks, such as run a bath or boil a kettle, which appear when a smartphone taps a sticker on the once familiar but now sometimes baffling object involved. Japan is pioneering the use of robotics in caring for the elderly. Examples include toys such as Paro, a furry seal used as a “therapy animal”, and Pepper, a humanoid robot deployed in hundreds of care homes to play games, hold childish conversations and demonstrate exercise moves.
But for most people in most parts of the world, the best that can be offered people with dementia at home and their carers is a daily knock on the door, or a phone call, like Ms Evans’s, and Post-it notes of helpful remindersto wash your hands, for example. So long as they are physically healthy, now is not the time, in many parts of the world, to contemplate sending someone with dementia into a care home. Many are operating strict isolation policies, letting no one in. And many have seen outbreaks of covid-19 infection. A study by academics based at the London School of Economics estimated that in a number of European countries, about half of covid19-related deaths have been in care homes.
Many carers of people with dementia who have been unfortunate enough to become infected with the virus see hospitalisation as a very last resort for their charges. Even Alzheimer’s Disease International, an advocacy group, reports in a position paper this month that “people over 80 who have other illnesses and need admission to hospital with covid-19 are least likely to benefit from going into hospital since their admission has associated risks.” The experience can be bewildering, and lead to delirium, a hallucinatory state of confusion and panic. “It’s pretty frightening for most people,” says Gill Livingston, professor of psychiatry of older people, at University College, London, “but even more frightening for them.” There is also the fear that, when it comes to triage—the selection of patients for scarce medical resources, the elderly with dementia will find themselves at the end of the queue, based on questionable assumptions about the patient’s underlying frailty and quality of life.
Besides the short-term dangers the virus has brought to those coping with dementia, there are fears it could do longer-term damage to efforts to improve care for the condition. One reason for this is shared with many physical maladies: that, during the emergency, people are wary of seeking diagnosis or help, for fear of infection, or of laying claim to health-care resources others need more urgently. Professor Livingston says that the “memory clinic” where she works decided to shut, as the doctors concluded “it was more risky to see people than for them not to have a diagnosis for a short period of time.” But the longer the delay goes on, the greater dangers people living with undiagnosed dementia pose to themselves, and perhaps others, if, say, through forgetfulness they start a fire, or continue to drive when they can no longer do so safely.
Scientific research into dementia has also been disrupted by the pandemic. Miia Kivipelto, a Finnish neuroscientist who led a pioneering study showing how changes in people’s ways of life could slow or arrest cognitive decline, has had to stop all the follow-up research, as it is impossible to conduct in a world of self-isolation. Similarly, Biogen, an American pharmaceutical company, has had to delay its attempt to gain approval for aducanamab, a potential treatment for Alzheimer’s. Besides the difficulty in conducting clinical trials, the company has suffered a covid-19 outbreak. So many Alzheimer’s drugs have failed that optimism about this one was at best cautious, but for some of those affected by the disease, it was a light at the end of a very long tunnel.
Before Covid-19, campaigners for dementia research and dementia care had reason to believe that they were making progress. Their argument that dementia is not an inevitable feature of ageing but a disability that deserves to be treated as such was widely accepted. So too was their case that dementia represents a real global emergency.
As life expectancies lengthen, especially in the developing world, the numbers of people with the condition will shoot up, to around 80m by 2030 and 150m by 2050. As population growth slows, there will simply not be enough people to care for them. No country has a good plan for how to deal with this problem, or how to finance the care of such large numbers of people. Optimists point to the current pandemic to argue that it shows how much can be done when the scale of an emergency is recognised. Perhaps more realistically, it has given yet another reason for dementia to slip down the list of global priorities.
Source: The Economist